The diagnosis of BBS is based on clinical findings. Consider the complete presentation and use your clinical judgment to diagnose BBS.2-7,9,13,14
Clinical features
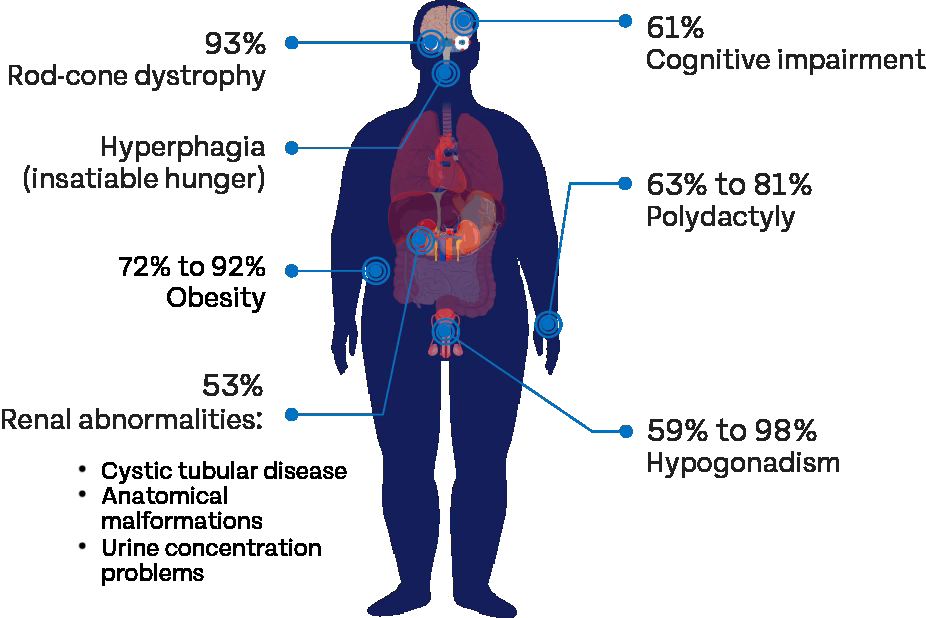
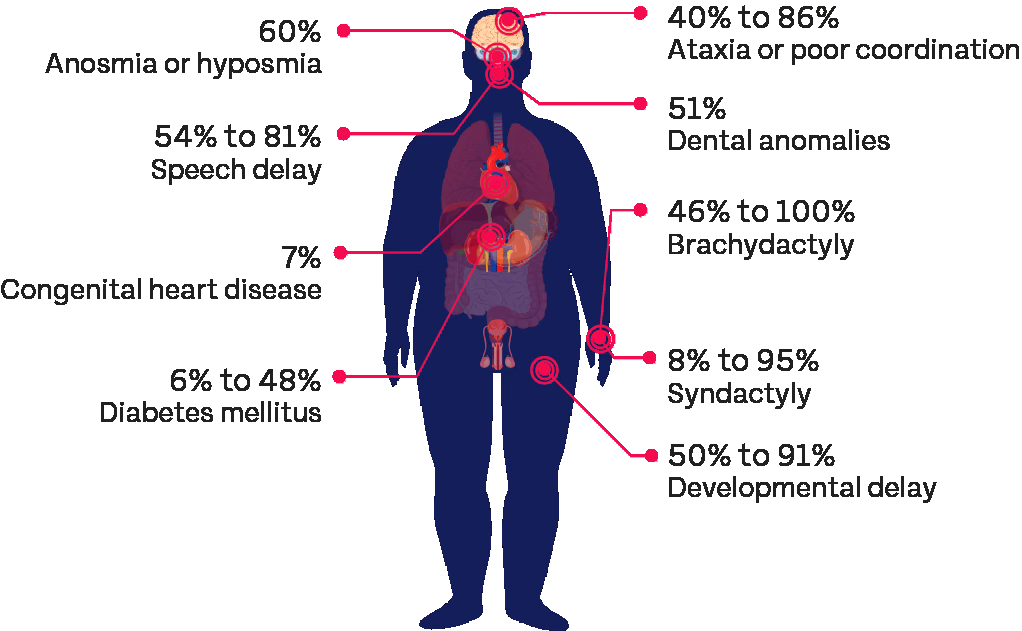
The presence of clinical features associated with BBS may vary, but can often include hyperphagia and early-onset, severe obesity, among others, such as visual impairment, cognitive impairment, renal anomalies, polydactyly, and hypogonadism.4,5,9,13,14
Most Common clinical features5,7,12
Other clinical features5,7
BBS, Bardet-Biedl syndrome.
Evolution of clinical features of BBS1-6,8,10-12,15,16
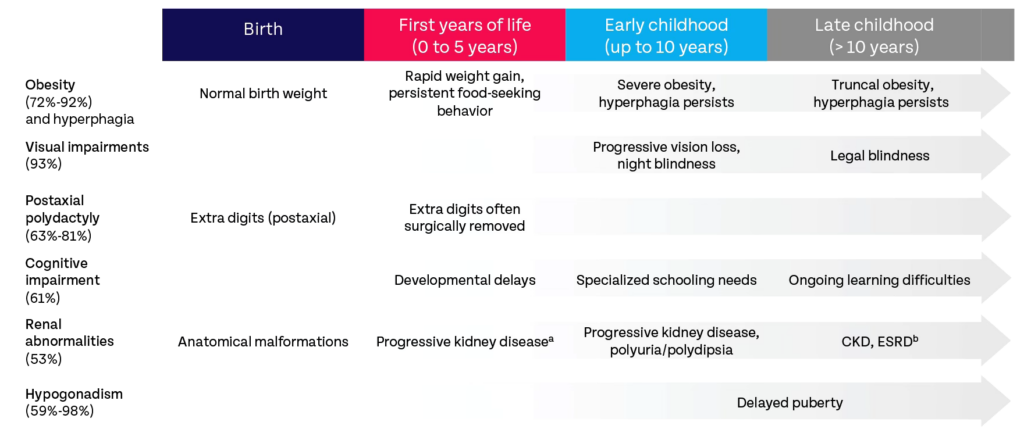
aPediatric patients with CKD stages 4 and 5 were diagnosed before age 5 years; patients either developed CKD in childhood or maintained normal or near-normal renal function into adulthood.
bIf polyuria is absent or overlooked, ESRD, which occurs at various ages from birth, may be the first renal manifestation.9
BBS, Bardet-Biedl syndrome; CKD, chronic kidney disease; ESRD, end-stage renal disease.11
Genetics
BBS is diagnosed clinically. Genetic testing can help provide additional evidence to support the diagnosis of BBS. BBS is clinically and genetically diverse; clinical features, genetics, patient history, and family findings should all be considered.4,5,7,9,13,14
Patient history and family findings
BBS, Bardet-Biedl syndrome; MC4R, melanocortin-4 receptor
References
- Agrawal H et al. Pediatr Rev. 2018;39(5):e21-e23.
- Beales PL, et al. J Med Genet. 1999;36(6):437-446.
- Castro-Sánchez S et al. J Med Genet. 2015;52(8):503-513.
- Forsyth R, Gunay-Aygun M. GeneReviews. Accessed February 21, 2024. https://www. ncbi.nlm.nih.gov/books/NBK1363
- Forsythe E, Beales PL. Eur J Hum Genet. 2013;21(1):8-13.
- Forsythe E, et al. J Am Soc Nephrol. 2017;28(3):963-970.
- Forsythe E, et al. Front Pediatr. 2018;6(23):1-8.
- Hooda AK, et al. Indian J Nephrol. 2009;19(3):112-114.
- Milani D, et al. Ital J Pediatr. 2014;40(1):33.
- Pomeroy J, et al. Pediatr Obes. 2021;16(2):e12703.
- Putoux A, et al. Pediatr Nephrol. 2012;27(1):7-15.
- Sherafat-Kazemzadeh R, et al. Pediatr Obes. 2013;8(5):e64-e67.
- Styne DM, et al. J Clin Endocrinol Metab. 2017;102(3):709-757.
- van der Valk ES, et al. Obes Rev. 2019;20(6):795-804.
- Vlahovic AM, Haxhija EQ. Pediatric and Adolescent Plastic Surgery for the Clinician. Springer; 2017:89-105.
- Weihbrecht K, et al. Med Res Arch. 2017;5(9):10.18103/mra.v5i9.1526.
